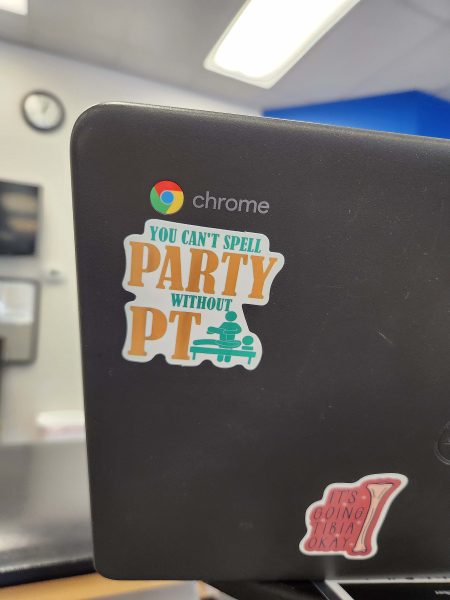
2024 was, physically, a long haul for me. First, I had a TKR (total knee replacement) in April. Then, in late July, when I was two weeks away from finishing physical therapy for my knee, I injured my ankle (same leg as the knee replacement) doing PT for my knee on a leg press machine. My ankle had significant, but not severe pain, so I bought an elastic sleeve and wore that to stabilize the joint. After two weeks, when the pain continued to increase, I made an appointment with my orthopedist.
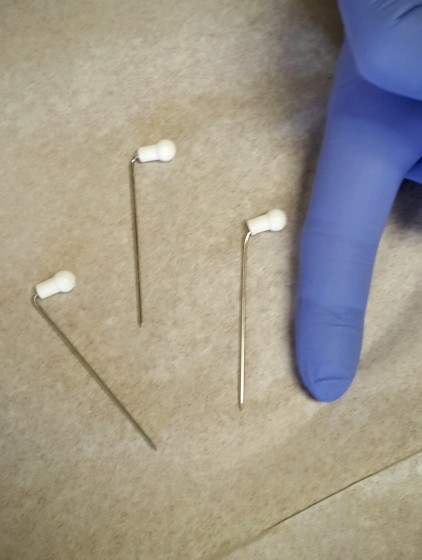
He ordered an x-ray, diagnosed the injury as a “severe posterior tibial strain,” and provided me with what he called a “strappy”–a very firm elastic sleeve. In the photo below, my foot enters at the top, my heel protrudes from the sock-like portion of the strappy on the left, and my toes extend through the opening on the right. The straps wrap all the way under, over, and around my ankle in opposite directions. Together, the straps and the sock portion of the strappy provided three layers of very firm support around my ankle, in every direction of ankle movement.


I was instructed to wear the strappy for a month and then to try walking without it. I had only minor pain with the strappy in place, but there wasn’t much improvement in my original pain level when I took the strappy off, so the doctor ordered an MRI. That revealed a partial tear in the tendon near my heel (the posterior tibial tendon). The prescription for that was to completely immobilize my ankle by wearing a boot for a month. After a month, I saw some improvement, but there was still significant ankle pain, so I wore the boot for another month. (If you’ve ever worn a boot, you know how much fun that was, right?) By then, my ankle didn’t hurt, but it felt very fragile–as if exertion might re-tear the tendon, so I went back to the strappy for another month. (BTW, during all of this, my knee felt great!)
I experimentally took the strappy off on Christmas Day and kept my activities at a low level for a week to test my ankle. Five months after injuring it, my ankle feels healed, but it’s incredibly weak, so it tires quickly. After all, for five months, it did very little work, having been supported by a variety of devices for that entire time. When the big snowstorm arrived on January 5, I pushed the snowblower for an hour-and-a-half after the first part of the storm and for another hour-and-a-half after the backside of the storm without pain in my ankle–probably because my snow boots provided support for my ankle.
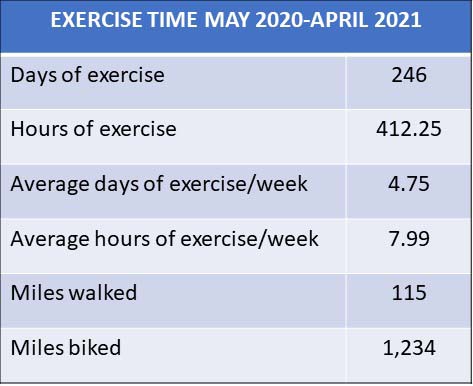
With the knee pain becoming severe in December 2023, then the TKR in April 2024, and then the July 2024 ankle injury that didn’t heal until December 2024, I’ve done minimal physical exercise for over a year! I don’t think I’ve ever been this weak or this out of shape in my life!
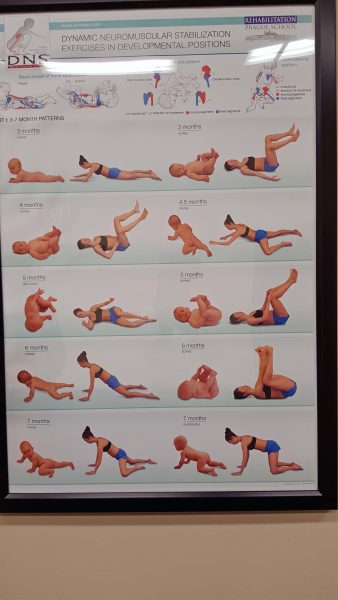
On January 1, I started walking for exercise again, and my ankle is becoming noticeably stronger. At this point, I can comfortably walk a mile outdoors before my ankle starts to protest with weak muscle pain. I’ve been told that: (1) a tendon tear does not heal to its original state; and (2) if my ankle was supported for 5 months, you add that time for the injury to heal–i.e., another 5 months. That will be Memorial Day.
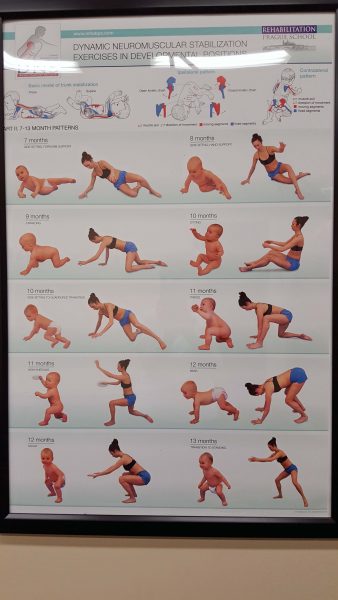
Meanwhile I’ve also started doing Pilates again and I’m looking forward to biking when the weather gets a little warmer–two activities I had to give up a year ago because of my knee pain. My doctor, my physical therapist, and my Pilates instructor all say it will take 4-6 weeks to see obvious improvement in my overall strength and fitness, and 8-12 weeks to reach the level I’m accustomed to having. Twelve weeks will be March 31. I can’t wait!
It feels wonderful to be active and even better to be pain-free. Hurray for me!
♫ Happy days are here again! ♫