My right knee has been bone-on-bone for nearly four years but, with gel injections in my knee every six months and an elastic sleeve to stabilize the joint, I managed to delay surgery until March 2024, when the February gel injection made no difference at all in my knee pain level. It was time to schedule a TKR—a total knee replacement.
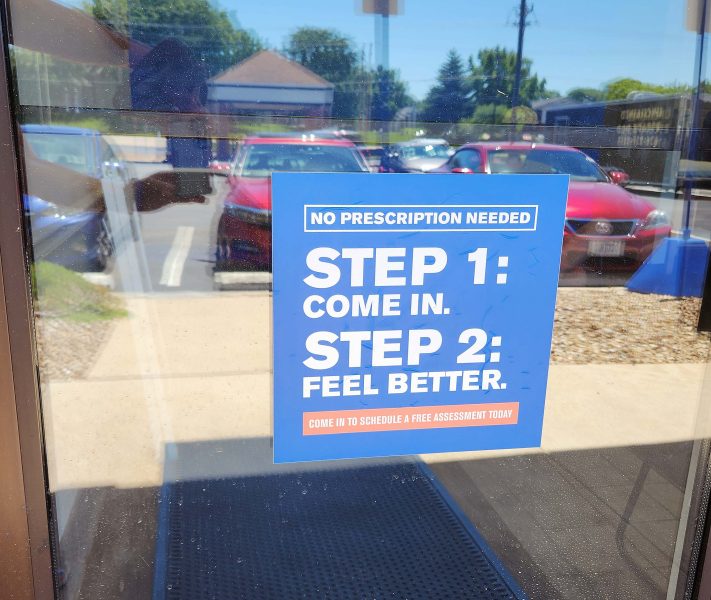
I made an appointment with my orthopedist to discuss the surgery and to set a date for the TKR. My only condition was that it had to be after the April 8 total solar eclipse. There was no way I was going to miss that!! Because I was having difficulty doing so many things—walking more than a half-mile, standing for more than 30 minutes, biking, Pilates, etc.—I decided to do physical therapy (PT) before my surgery to strengthen the muscles around my affected knee and to improve the healing process following the surgery. I’ve gone to Athletico for various types of PT in the past and have always enjoyed working with their outstanding staff. This time was no different. Their attitude begins at the front door.
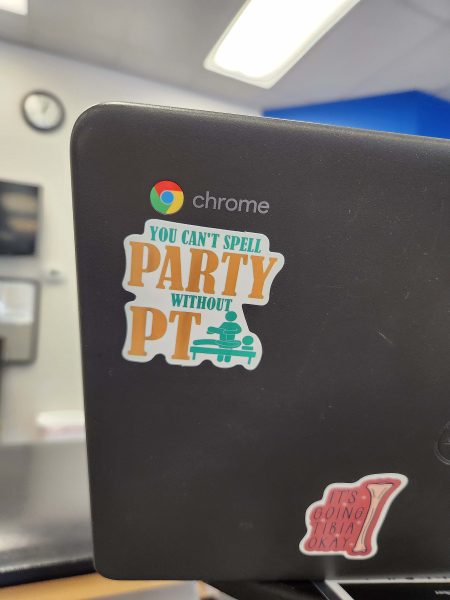
More detail is provided on Sarah’s (my therapist) laptop.
The pen mug at the check-in desk reminds patients and staff why we’re there.

The mood indicator lets us know how the staff is feeling

In the 22 weeks I worked with Sarah, I only saw one mood change. I don’t remember what it was, but it amounted to “It’s a ho-hum kind of day.” Every other day was “happy,” and that’s the atmosphere you can feel when you’re there.
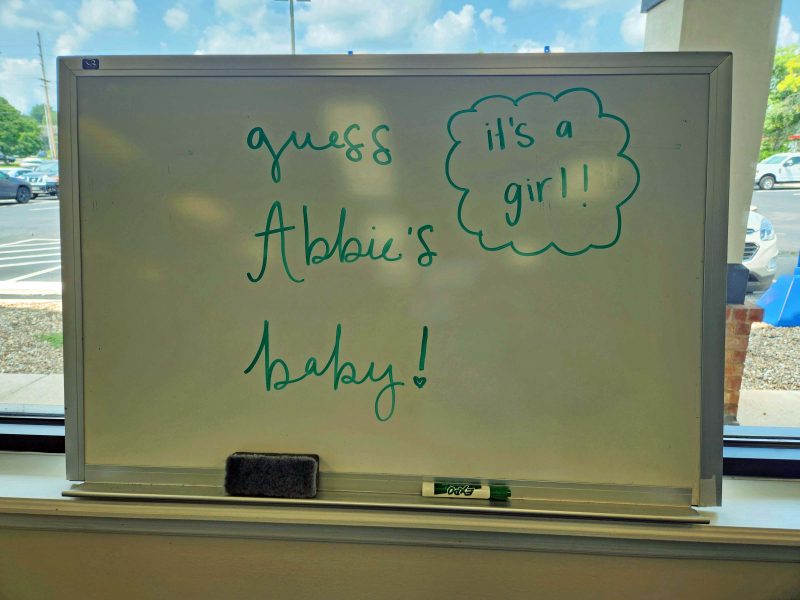
Most days, there’s some topic under discussion, and everyone—staff and patients—joins in while the therapy continues. One day, for example, the staff was planning a potluck lunch for themselves and thought it would be fun if each staff member brought a food item that began with the same letter as their first name. That was an entertaining discussion, with everyone contributing ideas—some realistic, some hilarious! On another day, during the Olympics, the TV was on. When Simone Biles performed, therapy stopped temporarily while we all watched her, then cheered for her. Abbie, one of the therapists, was pregnant, and was going to learn the gender of her baby at her next OB visit. For a few weeks before Abbie’s appointment, a whiteboard propped near the entrance invited everyone to “Guess Abbie’s Baby.” Staff, patients, and visitors (usually patients’ drivers) could vote for “boy” or “girl.” “Boy” outnumbered “girl” by about 6-1. I voted with the minority for a girl. After Abbie’s visit with her OB, the board showed the results.
Sarah, my therapist, was fun to work with. One of my friends sent me some goofy goggles to share with her, and Sarah was willing to go with them for a photo op.

The general consensus among my doctor, my physical therapist, and my friends who have had TKR surgery was that the first two months after the surgery are “tough,” but things get much better in the third month. I didn’t get many specifics about what “tough” included, and now I know why. As Forrest Gump said, “That’s all I have to say about that”—just like all those people I talked with.
My first post-surgical PT session was scheduled three days after my surgery. It was very painful, due to the swelling and the surgical pain. During that session, I had to keep reminding myself that I had actually liked Sarah a lot at my pre-surgical session six days earlier. With Sarah’s expertise, eight weeks of PT prior to the surgery, and my determination, I made rapid post-surgical progress. I did my PT exercises every day—before and after surgery—for a total of 22 weeks, with only a few (11 of 154 days) exceptions.
Thanks to all the PT I did, I needed a walker for only four days, then walked with a cane for a week, and then walked on my own. When I had my one-month post-surgical visit with my orthopedist, he and his staff were amazed that I was walking on my own without a limp. They had the same reaction to my physical progress at my next visit, six weeks later. They told me that, at the 10-week point, many people are still walking with a cane (or at least limping); some still take pain meds; most don’t have the range of motion or the strength in their knee that I do; and most are still doing stairs one step at a time. Unbelievable! I’m so glad I did pre-surgery PT!
The two best tools I bought for my recovery were: (1) an ice/compression machine; and (2) a pedal exerciser. The ice/compression machine replaced the CPM (continuous passive motion) machine that TKR patients formerly needed. Basically, it’s an ice pack version of a heating pad attached to a six-pack-size cooler with a water/ice reservoir and a motor that circulates the ice water from the reservoir to provide the added benefit of intermittent forced-air compression. The ice and compression kept the swelling—and therefore, the pain—down, and walking plus PT kept my knee flexible. At first, my knee couldn’t bend enough for the top of the stroke on my stationary bike, but sitting on a chair to use the pedal exerciser in a more recumbent position was an easy way to keep my knee flexible whenever I needed it during the day and, unfortunately, the night.

Sarah and my orthopedist used measurements and physical evaluations to determine my progress; I set my own goals. Success for me included:
- Walk a mile outdoors one month after surgery. I did that and walked two miles on the neighborhood streets three weeks later. On my first outdoor walk after my surgery, I only made it to the second house past ours. I went a little farther each day until I could walk two miles.
- Bike at least 10 miles three months after surgery. I had to wait two months to bike because my knee had to heal enough to support me just in case my bicycle tipped and forced me to throw my leg out to the side to keep from falling. If I injured my knee before it was sufficiently healed, the chances were good that I’d need surgical treatment to repair it. At two months, I rode 7 miles on my bicycle, and at the three-month mark, I rode 15 miles.
- Achieve at least 135o of flexion in my new knee by the end of my PT sessions. There’s a limit to how far a mechanical replacement knee joint can be flexed. The PT goal is 120o-130o. The normal range of flexion for a natural knee is 120o-150o; about 145o is average. At my last PT session, Sarah prepared her report for my doctor and measured my knee flexion at 141o. I took that good news home to Ted, and we went out for medium-sized (not small) chocolate-dipped DQ cones to celebrate.
I am so thankful for all the people—the doctors, the nurses, Sarah, other PT patients, friends, family, and especially Ted, for getting me through this. I couldn’t have done it without all of you—especially during those first two months! It’s great to move without knee pain.